Did you know nearly 50% of adults in the United States over age 30 have some form of gum disease? This widespread condition often develops quietly, showing little warning until serious damage occurs. Understanding what is gum disease isn’t just about your gums—it’s essential for protecting your teeth, your oral health, and your overall wellbeing.
A Startling Reality: Why Understanding What is Gum Disease Matters
Gum disease isn’t simply about having swollen gums—it’s a progressive problem that can lead to tooth loss, bone loss, and even impact your heart and overall health if left untreated. Both gum disease and periodontal disease describe inflammation and infection of the gum tissue and supporting structures. What’s alarming is that many people aren’t aware of the subtle signs that signal the early stage of gum disease.
For preventive care to be effective, it’s crucial to know the risk factors, understand the symptoms of gum disease, and realize that it can affect anyone, even those who brush and floss daily. Poor oral hygiene, smoking, certain illnesses, or genetics can all tip the balance. By educating yourself, you’re not just saving your smile—you’re safeguarding your overall oral health.
Opening Statistics: The Prevalence and Impact of Gum Disease
According to recent studies, half of American adults show symptoms of gum disease, making it one of the most common chronic diseases worldwide. The early stage, known as gingivitis, is reversible. However, if left untreated, it can progress to periodontitis, which affects the gum line, causes bone loss, and can eventually require advanced treatments like bone grafts.
The economic and health impact is significant. Gum disease leads to millions of lost teeth annually, causing both emotional and financial strain. Furthermore, studies now link periodontal disease to serious illnesses such as diabetes and heart disease, making awareness and prevention more important than ever.

What You'll Learn About What is Gum Disease
Definition and stages of gum disease
Differences between gum disease and periodontal disease
Key symptoms of gum disease
Risk factors for developing gum disease
Prevention and treatment options for gum disease
How gum disease affects overall oral health
Defining What is Gum Disease: The Basics of Periodontal Disease
What is Gum Disease and How Does it Begin?
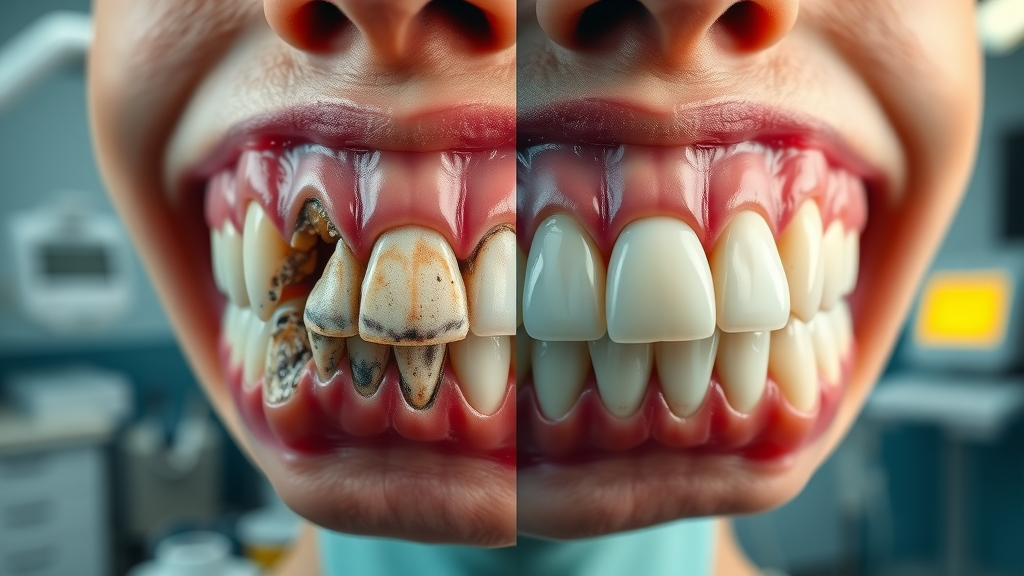
Gum disease, medically known as periodontal disease, begins when sticky bacteria called plaque build up along the gum line and teeth. Without regular oral hygiene—brushing, flossing, and professional cleaning—this plaque hardens into tartar, irritating the gum tissue and triggering inflammation. The earliest form of gum disease is called gingivitis; it’s marked by red, swollen gums that may bleed slightly during brushing or flossing.
If not addressed, gingivitis can lead to periodontitis, which is a more advanced form of gum disease. During this stage, the gums pull away from the teeth, creating pockets where bacteria thrive. Over time, these bacteria can damage the bone supporting your teeth, leading to bone loss, receding gums, and even tooth loss. The process is typically painless, so you might not know it’s happening until significant damage has occurred.
Gum Disease vs. Periodontal Disease: Understanding the Terms
The terms “gum disease” and “periodontal disease” are often used interchangeably. However, gum disease refers broadly to all inflammatory conditions affecting the gums, while periodontal disease specifically describes inflammation affecting not just the gums but also the structures that support your teeth, including the bone.
Gingivitis is the earliest, mildest form of gum disease and only involves gum tissue. Periodontitis is more severe, involving both the gum and the underlying bone. As periodontitis progresses, damage can become permanent without professional intervention. Knowing these distinctions helps you understand the seriousness of symptoms you may experience and underscores the importance of early detection.
Understanding the progression from gingivitis to periodontitis is crucial, especially since advanced cases can result in tooth loss and the need for restorative solutions. For those interested in how missing teeth can be addressed after severe gum disease, explore the benefits and process of dental implants as a long-term solution for restoring both function and aesthetics.
Recognizing Symptoms of Gum Disease: Early Warning Signs
Top Symptoms of Gum Disease
Identifying the symptoms of gum disease at an early stage is vital for effective treatment and recovery. Common symptoms you should watch for include:
Red or swollen gums: Healthy gums are pink and firm. Inflammation is an early sign you might be experiencing gingivitis or progressing toward periodontitis.
Bleeding during brushing or flossing: While occasional bleeding can happen, persistent bleeding is a warning sign.
Bad breath (halitosis): Ongoing bad breath can result from increased bacterial activity in infected gums.
Receding gum lines: If your teeth suddenly appear longer, or you can see more of your tooth’s root, your gums may be pulling away due to chronic inflammation.
Loose teeth: As the gum tissue and supporting bone weaken, teeth may become mobile or shift.

Symptoms of Gum Disease vs. Symptoms of Periodontal Disease
While early gum disease (gingivitis) primarily affects the gums—causing redness, swelling, and bleeding—periodontal disease presents more alarming symptoms. As infection spreads deeper, you’ll notice gum recession, persistent bad breath, pus formation, loose teeth, changes in how teeth fit together, and even noticeable bone loss.
Not all forms of gum disease include every symptom, which complicates self-diagnosis. What’s common is that patients often delay treatment because discomfort is minimal at first. Recognizing differences, even between mild gingivitis and advanced periodontitis, is your best defense against future tooth loss or damage to the gum line.
Risk Factors for Gum Disease: What Puts Your Oral Health at Stake
Major Risk Factors and Contributors
Several risk factors can make you more susceptible to developing gum disease, even if you practice good oral hygiene. Key factors include:
Poor oral hygiene
Smoking or tobacco use
Genetics
Chronic illnesses (e.g., diabetes)
Certain medications
oral health
Understanding the Role of Oral Health in Preventing Gum Disease
Good oral health habits—like brushing and flossing consistently, using mouthwash, eating a balanced diet, and attending regular dental check-ups—are your best defense against gum disease. Thorough daily cleaning helps remove plaque before it calcifies into tartar, which can only be scrubbed away during a professional cleaning by a dentist or dental hygienist.
Commitment to oral hygiene reduces the bacterial load in the mouth, lessening inflammation and risk for both minor and severe periodontal disease. A strong oral care routine, combined with lifestyle changes such as quitting smoking, gives you the best chance of achieving a lifetime of healthy teeth and gums.
Animated Overview: What is Gum Disease and How it Progresses (See accompanying video on our website for a visual guide.)
Stage by Stage: How Gum Disease Progresses to Advanced Periodontitis
Gingivitis: The First Stage of Gum Disease
The earliest stage of gum disease is gingivitis. It develops when plaque—an invisible, sticky film of bacteria—builds up on teeth and inflames the gums. Symptoms include minor swelling, tenderness, and bleeding during brushing. Gingivitis is typically painless and reversible with good oral hygiene and regular professional care.
If ignored, the infection can advance beyond the gum tissue, threatening deeper structures and signaling progression to a more dangerous phase of gum disease.
Progression to Periodontitis and Advanced Periodontitis
Untreated gingivitis can turn into periodontitis, where chronic inflammation destroys both gum tissue and the underlying bone that holds your teeth in place. Gums may recede, pockets form around teeth, and bone may start to erode—making the condition harder to treat.
As advanced periodontitis establishes itself, tooth mobility increases and tooth loss becomes a real threat. Treatments in these stages often require scaling and root planing, antibiotics, and sometimes surgical procedures like gum or bone grafts. Recognizing it early and seeking help is essential, as Dr. Walsh says:
"Early intervention for gum disease can preserve your smile and prevent extensive damage." - Dr. Brian Walsh

How Gum Disease Affects Overall Oral Health
The Link Between Gum Disease and Systemic Health
Gum disease doesn’t just threaten your teeth and gums. Mounting scientific evidence suggests chronic inflammation in the mouth is closely tied to several serious health conditions. Untreated gum infections have been linked to:
Heart disease
Diabetes complications
Pregnancy and birth outcomes
Respiratory diseases
taking care of your gums is a vital part of maintaining your general health
Diagnosing Gum Disease: The Importance of Regular Dental Visits
What to Expect at Your Dental Appointment
Early diagnosis is the key to preventing irreversible damage from gum disease. During a regular dental visit, your dentist or dental hygienist will:
Check for swelling, bleeding, receding gums, and tartar buildup
Measure the depth of gum pockets using a periodontal probe
Take dental x-rays to assess bone loss
Key Tools and Tests for Detecting Periodontal Disease
In addition to visual exams, several diagnostic tools help dentists detect and monitor periodontal disease progression:
Periodontal probing: Measures pocket depths around teeth. Deeper pockets often mean more severe disease.
Digital x-rays: Reveal changes in bone structure and possible bone loss around tooth roots.
Bacterial culture tests: Identify specific pathogens contributing to infection.

Stages of Gum Disease vs. Key Symptoms and Recommended Treatments |
||
Stage |
Symptoms |
Recommended Treatments |
|---|---|---|
Gingivitis |
Red, swollen gums; bleeding when brushing |
Improved brushing/flossing; regular dental cleanings; antibacterial rinses |
Early Periodontitis |
Gum recession; mild bone loss; persistent bad breath |
Scaling and root planing; possible antibiotics; personalized oral hygiene |
Advanced Periodontitis |
Deep gum pockets; significant bone loss; loose or shifting teeth |
Surgical intervention; bone grafts; ongoing periodontal therapy |
Treating Gum Disease: From Home Remedies to Professional Care
How to Fix Gum Disease at Home
For mild cases of gum inflammation, especially those in the early stage (gingivitis), consistent home care can make a major difference. Helpful strategies include:
Improved oral hygiene routines: Brush at least twice daily using a fluoride toothpaste. Floss carefully to remove plaque and debris between teeth and along the gum line.
Antibacterial mouthwashes: These can reduce harmful bacteria and control infection.
Diet and lifestyle changes: Eating more fruits and vegetables, reducing sugar intake, and quitting smoking all reduce your risk for progression.

Professional Treatments for Gum Disease and Periodontal Disease
When gum disease progresses beyond the mild stage, dental professionals offer advanced treatments, such as:
Scaling and root planing: Deep cleaning below the gum line to remove plaque and tartar buildup and smooth root surfaces for healing.
Antibiotic therapies: Local or systemic antibiotics may be prescribed to target persistent infections.
Surgical interventions: Procedures like flap surgery, soft tissue grafts, or bone grafts repair gum tissue and underlying structures compromised by severe periodontal disease.
Preventing Gum Disease: Essential Oral Health Habits
Daily Practices to Prevent Gum Disease
Developing a preventive mindset is the best way to guard against gum disease and safeguard your oral health for life. Core practices include:
Correct brushing and flossing techniques: Brush gently in circular motions along the gum line and floss daily to remove plaque your toothbrush can’t reach.
Routine dental check-ups: Schedule professional cleanings and exams at least twice a year. Your dentist can spot and treat issues before they escalate.
Diet tips for healthy gums: Choose wholesome foods rich in vitamins and minerals, especially vitamin C, which supports gum repair. Hydrate well and minimize sugary snacks that fuel harmful oral bacteria.
periodontal disease
People Also Ask: Common Questions About What is Gum Disease
Can I live a long life with gum disease?
Yes, many people live with gum disease, especially in its milder forms, for many years. However, without treatment, gum disease can progress and impact overall health and longevity by increasing risks of related systemic conditions.
How to fix gum disease at home?
While mild gum disease (gingivitis) can sometimes be managed at home with improved oral hygiene and regular brushing/flossing, moderate to severe cases require professional treatment. Simple daily care is vital but may not be sufficient alone.
What antibiotics are used for gum disease?
Dentists may prescribe antibiotics such as doxycycline, metronidazole, or amoxicillin for gum disease, especially for periodontal infections not controlled by cleaning alone. Always consult a dental professional before starting antibiotics.
What is the main cause of gum disease?
The main cause of gum disease is plaque buildup—a sticky film of bacteria on teeth and gums. If not removed through regular dental care, this plaque can irritate gum tissue and lead to gum disease.
FAQs About What is Gum Disease
Is gum disease reversible? Early-stage gum disease (gingivitis) is reversible with consistent brushing, flossing, and professional dental cleanings. Advanced stages require more intensive treatments.
Can children get gum disease? Yes, children can develop gingivitis, though severe forms are more common in adults. Good oral habits early can prevent lifelong issues.
What is the difference between gingivitis and periodontitis? Gingivitis is inflammation limited to the gums and is reversible. Periodontitis is a deeper infection involving bone loss and tissue destruction, requiring professional care.
How often should I visit the dentist to prevent gum disease? Most people benefit from check-ups every six months, but your dentist may recommend more frequent visits based on your personal risk factors.
Does gum disease always cause tooth loss? No, not always. With early intervention and diligent care, tooth loss can often be prevented even in those at higher risk.
Key Takeaways: What is Gum Disease and How to Protect Your Oral Health
Gum disease is common but preventable with routine care
Early detection dramatically reduces risk of serious complications
Healthy oral habits and regular dental visits are essential
Conclusion: Take Charge of Your Oral Health and Prevent Gum Disease
Don't wait for symptoms – invest in preventive care for a bright, healthy smile.
If you’re ready to take your oral health to the next level, consider how a comprehensive approach to dental care can make a lasting difference. At Johnstown Dental Care, we believe in supporting your smile through every stage of life, from preventive checkups to advanced restorative solutions. For a broader look at how our team can help you and your family achieve optimal dental wellness, discover the full range of family dental services and patient-focused care we provide. Your journey to a healthier, more confident smile starts with the right information and a trusted dental partner by your side.
Contact Johnstown Dental Care for Gum Disease Prevention and Treatment
Johnstown Dental Care 370 West Coshocton St. Johnstown, OH 43031
Phone: (470) 967-6046
Website: www.johnstowndentalcare.com
Proudly Serving: Johnstown, New Albany, Granville, Alexandria, Pataskala, and surrounding areas in Licking County, Franklin County, and Delaware County.
Gum disease, also known as periodontal disease, is a common condition affecting the tissues surrounding the teeth. It typically begins with gingivitis, characterized by red, swollen gums that may bleed during brushing or flossing. If left untreated, it can progress to periodontitis, leading to gum recession, bone loss, and potentially tooth loss. Understanding the causes, symptoms, and preventive measures is crucial for maintaining optimal oral health.
For a comprehensive overview of gum disease, including its symptoms, causes, and treatment options, refer to the Mayo Clinic’s article on Periodontitis - Symptoms and causes. Additionally, the Centers for Disease Control and Prevention provides valuable statistics and information on the prevalence and impact of gum disease in their Gum Disease Facts page. These resources offer in-depth insights into gum disease and strategies for prevention and treatment.
 Add Row
Add Row  Add
Add 



Write A Comment