Have you ever felt your mouth suddenly go parched, even when you’ve had enough to drink? Dry mouth—known medically as xerostomia—affects millions each year, causing discomfort and increasing your risk for dental issues. Why do I have a dry mouth? This guide pulls back the curtain on the surprising frequency, underlying causes, and practical solutions for dry mouth, so you can take charge of your oral health and find real relief.
Startling Facts: The Hidden Prevalence of Dry Mouth
"Did you know that up to 30% of adults experience dry mouth symptoms at some point in their lives? Yet, many cases remain undiagnosed."

What You'll Learn About Why Do I Have a Dry Mouth
The medical definition of dry mouth and why do I have a dry mouth
Causes and risk factors affecting salivary glands
Connections between dry mouth, health care, and oral health
Treatment for dry mouth and how a care provider can help
Preventative strategies to maintain health care of your oral cavity
Defining Dry Mouth: What Is Dry Mouth and Why Do I Have a Dry Mouth?
Dry mouth is a condition where you feel dry or sticky in your mouth due to a lack of saliva. Also called xerostomia, it leads to discomfort, difficulty swallowing or tasting food, and can even affect how you speak. If you find yourself asking, “Why do I have a dry mouth?,” you’re not alone. The sensation typically happens when your salivary glands don’t produce enough saliva to keep your mouth moist.
While everyone occasionally wakes up with a dry mouth or feels parched after a salty meal, persistent symptoms can signal an underlying health condition, side effect from medication, or lifestyle issues such as dehydration. The importance of saliva goes beyond just keeping your mouth wet—it plays a major role in protecting teeth, supporting digestion, and maintaining overall oral health. Discovering the cause of your dry mouth can be a crucial step toward better health and comfort.
Comparison of Wet Mouth vs Dry Mouth: Symptoms, Causes, and Impact on Oral Health |
||
Feature |
Wet Mouth (Healthy) |
Dry Mouth |
|---|---|---|
Symptoms |
Mouth feels moist, normal taste sensation, easy to chew/swallow |
Sticky or parched feeling, altered taste, cracked lips, difficulty chewing/swallowing |
Main Causes |
Adequate saliva from healthy salivary glands, good hydration, balanced health |
Medication side effect, dehydration, salivary gland disorders, health conditions like diabetes/Sjögren’s syndrome |
Oral Health Impact |
Protects against tooth decay, supports digestion, prevents gum disease |
Increases risk of tooth decay, gum disease, bad breath; oral infections more likely |
Salivary Gland Function: The Key to Oral Health and Dry Mouth
How Salivary Glands Work and Their Link to Why Do I Have a Dry Mouth
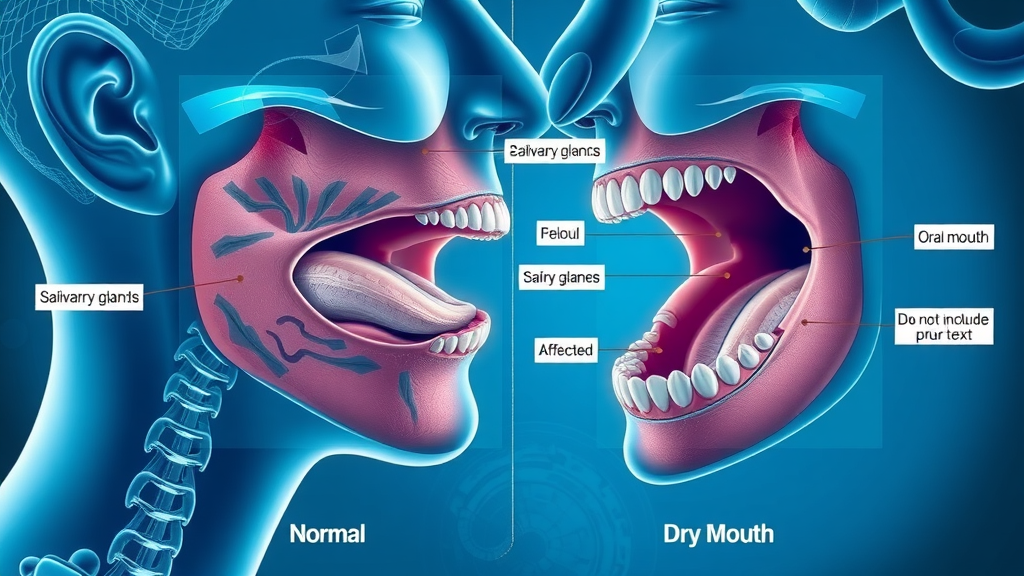
Your salivary glands are vital for keeping your mouth healthy and moist. There are three major pairs of glands—the parotid, submandibular, and sublingual—that constantly work to produce and release saliva. Saliva has key roles: it helps you chew and swallow, neutralizes acids to protect tooth enamel, rinses away food particles, and delivers immune defense against bacteria.
When these glands are functioning normally, your mouth stays moist and comfortable. However, when they slow down or are blocked, you may suddenly notice your mouth feels dry, you get thirsty more often, and eating or speaking becomes a challenge. This is often the root answer to, "Why do I have a dry mouth?"—something has interrupted your glands’ ability to supply enough saliva. If saliva production drops below a certain point, you start experiencing dry mouth symptoms like cracked lips, sore throat, or even trouble tasting foods.
Salivary Gland Disorders: Understanding the Causes Behind Dry Mouth
Problems with salivary glands aren’t always obvious. They can be affected by infections, blockages (such as salivary stones), or autoimmune disorders like Sjögren’s syndrome, which actually attack the glands directly. Even radiation treatments for head and neck cancer can permanently impair their function.
The result? Chronic dry mouth, where your mouth is consistently unable to stay moist on its own. Often, a side effect from prescription medications or a sign of a deeper health condition, gland problems should never be ignored. If you notice swelling, pain, or long-term dryness, it’s time to involve a health care provider and seek the right diagnosis. Early intervention can prevent more serious oral health issues down the road.
In some cases, addressing dry mouth may also involve restorative dental procedures, especially if tooth surfaces have been compromised. For example, dental bonding can help repair minor damage caused by persistent dryness and protect your teeth from further decay.
Common Causes: Why Do I Have a Dry Mouth?
Many people with dry mouth are surprised to learn how common and varied the causes can be. Identifying what’s affecting your saliva is crucial. Here are some primary reasons you might feel dry or experience persistent mouth symptoms:
Medication side effects: Hundreds of medications list dry mouth as a possible side effect. These include antidepressants, blood pressure medications, antihistamines, and more.
Health conditions: Diseases like diabetes or Sjögren’s syndrome can disrupt saliva production by attacking glands or altering body chemistry.
Dehydration and lifestyle habits: Not drinking enough water, consuming excessive caffeine or alcohol, tobacco use, and mouth breathing all contribute to dryness.
Impact of aging: Older adults often experience reduced saliva flow due to medication use or changes in their bodies as they age.
Recognizing the specific cause behind why do I have a dry mouth can help you and your care provider choose the most effective treatment for dry mouth, protect your oral health, and prevent other related problems.
Diagnosing Dry Mouth: When to See Your Health Care Provider
Dry Mouth and Related Health Care Factors
Professional evaluation is key in managing persistent or chronic dry mouth. A doctor or dentist will consider your medical history, medications, and any associated symptoms you might have. Sometimes, your health care provider can quickly pinpoint why your mouth is dry, especially if it lines up with certain medical conditions or therapy side effects.
Don’t ignore symptoms like ongoing dryness, trouble swallowing, a burning sensation, or mouth sores. Dry mouth symptoms may start mildly but increase in severity or signal a deeper underlying problem. It’s especially important to seek help if your condition affects eating, speaking, or oral hygiene, as neglect can lead to gum disease or tooth decay. Your care provider helps connect the dots to possible systemic illness or emerging health issues, ensuring early intervention for your comfort and wellbeing.
Tests and Examinations by Your Health Care Provider
During your appointment, expect a thorough oral exam. Your provider may check the moisture in your mouth, inspect your glands for swelling or tenderness, and ask about related symptoms. Common tests for dry mouth include measuring saliva flow, bloodwork (for autoimmune diseases), or imaging studies to detect blockages or gland inflammation.
Sharing a full list of your medications and being honest about habits (like caffeine or tobacco use) is vital for accurate diagnosis. In some cases, referral to a dentist, ENT specialist, or rheumatologist is necessary for complex causes. The right diagnosis unlocks a treatment for dry mouth that addresses both relief and prevention, helping restore your oral health and comfort.

The Impact of Dry Mouth on Oral Health and Tooth Decay
How Dry Mouth Leads to Tooth Decay and Other Oral Health Issues
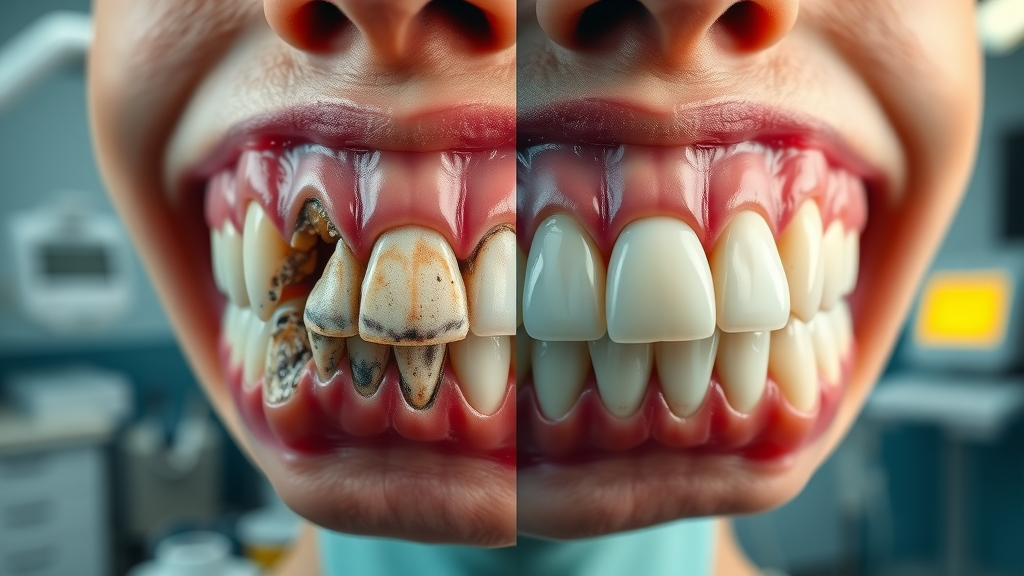
Saliva is the mouth’s frontline defense against tooth decay and gum disease. It continually washes away food particles, neutralizes harmful acids, and helps protect the enamel on your teeth. When you have dry mouth, your defenses are weakened, allowing bacteria to multiply, acids to linger longer, and food debris to build up.
The result? A much higher risk of cavities, oral infections like thrush, sore or cracked lips, and even chronic bad breath. Without enough saliva, your teeth and gums suffer, and the cycle of discomfort continues. For those wondering, “Why do I have a dry mouth that keeps affecting my teeth?,” it’s because the protective properties of saliva are deeply linked to maintaining a healthy, comfortable mouth.
Preventive Health Care Tips for Managing Dry Mouth
Prevention starts with addressing risk factors and building good oral hygiene habits. Drinking more water throughout the day is a simple but effective step. Using fluoridated toothpaste and visiting your dentist regularly can catch early signs of tooth decay before they become major problems.
Avoiding tobacco, limiting caffeine and alcohol, and choosing sugar-free gums or lozenges all encourage saliva flow. Special oral care products—like mouth rinses designed for dry mouth—make a big difference in comfort and health. If your symptoms persist or worsen, a health care provider can recommend stronger solutions or investigate deeper causes, ensuring you stay ahead of potential oral complications.
Explainer: How Salivary Glands Affect Dry Mouth and Oral Health
Treatment for Dry Mouth: Options for Relief
Over-the-Counter and Professional Treatment for Dry Mouth
Plenty of treatment for dry mouth options are available, from pharmacy products to care provider interventions. Over-the-counter remedies include artificial saliva sprays, gels, and mouthwashes made specifically to relieve dryness and create a lasting moist feeling. Some toothpaste brands include additional lubricants, while lozenges or chewing sugar-free gum can stimulate saliva flow naturally.
For severe or chronic dry mouth, your doctor or dentist may prescribe medications that prompt your glands to increase saliva production. You may also need to change medications if they’re a known side effect culprit. Sometimes, treating the underlying problem (like diabetes or autoimmune diseases) can directly reduce dry mouth symptoms. A combination of therapies is often the most effective path to relief, especially for people experiencing prolonged or stubborn symptoms.
Home Remedies and Lifestyle Changes to Address Dry Mouth
Simple changes in daily life can bring big relief from dry mouth symptoms. Sipping water frequently is one of the best habits for keeping your mouth healthy and wet. Avoiding salty, spicy, or overly sugary foods can prevent further mouth irritation, while a balanced diet with moisture-rich foods (like fresh fruits and vegetables) keeps you hydrated from the inside out.
Good oral hygiene is non-negotiable—brushing with a soft-bristled brush, flossing daily, and using alcohol-free mouth rinses go a long way. Consider investing in a humidifier if you live in a dry climate or find your mouth dry at night. And remember, minimizing caffeine and alcohol, plus quitting tobacco, can transform your symptoms. Quick action and consistent self-care, combined with professional advice from your care provider, offer real hope for those battling dry mouth.

When to Contact Your Care Provider About Dry Mouth
Persistent symptoms despite self-care
Signs of tooth decay or oral infections
Difficulties with eating or speaking
Swollen or tender salivary glands

People Also Ask: Common Questions About Why Do I Have a Dry Mouth
How do you get rid of a dry mouth?
Answer: There are several ways to get rid of a dry mouth, including staying hydrated, using saliva substitutes, avoiding caffeinated and alcoholic drinks, maintaining good oral hygiene, and consulting with your health care provider for personalized treatment.
What is a dry mouth a symptom of?
Answer: Dry mouth is often a symptom of underlying issues such as medication side effects, dehydration, autoimmune diseases like Sjögren’s syndrome, or problems with the salivary glands.
What are you lacking if you have a dry mouth?
Answer: Most commonly, dry mouth results from a lack of adequate saliva production which may be due to dehydration, nutritional deficiencies, or malfunctioning salivary glands.
Why is my mouth so dry even after drinking water?
Answer: If your mouth remains dry despite adequate water intake, it could be due to chronic health conditions, persistent medication side effects, or underlying salivary gland issues requiring professional attention.
Expert Q&A: Health Care Providers Discuss Causes and Treatment for Dry Mouth
Tips and Lists: How to Prevent and Manage Dry Mouth
Schedule regular health care check-ups
Use oral health products designed for dry mouth
Practice effective oral hygiene daily
Avoid tobacco and reduce alcohol consumption
Include moisture-rich foods in your diet

FAQs: Quick Answers to Why Do I Have a Dry Mouth
What medications most commonly cause dry mouth? Antidepressants, antihistamines, blood pressure drugs, decongestants, and muscle relaxants are among the most common.
Can stress lead to dry mouth? Yes. Stress and anxiety can lower saliva production, leading to temporary or persistent dryness.
Is dry mouth reversible? In many cases, yes—if you address the underlying causes, improve hydration, or modify medications with your provider’s help.
How does dry mouth affect tooth decay? Lacking saliva means bacteria and acids can damage teeth more easily, raising your risk of cavities and gum disease.
Key Takeaways: Why Do I Have a Dry Mouth
Understanding causes can help you seek effective treatment for dry mouth
Regular health care and oral health check-ups can prevent complications
Consult with your care provider for persistent or severe dry mouth symptoms
Conclusion: Taking Charge of Your Oral Health and Finding the Right Treatment for Dry Mouth
"Recognizing dry mouth early and working with your health care provider ensures optimal oral health and overall well-being."
If you’re interested in exploring more comprehensive solutions for restoring your smile and oral function, especially if dry mouth has led to tooth loss or significant dental issues, consider learning about advanced restorative options. Our overview of dental implants and their benefits can help you understand how modern dentistry addresses both function and aesthetics, empowering you to take the next step toward lasting oral health.
Contact Johnstown Dental Care for Expert Treatment on Dry Mouth
Johnstown Dental Care
370 West Coshocton St.
Johnstown, OH 43031
Phone: (470) 967-6046
Website: www.johnstowndentalcare.com
Proudly Serving: Johnstown, New Albany, Granville, Alexandria, Pataskala, Licking County, Franklin County, and Delaware County residents.
Dry mouth, or xerostomia, can result from various factors, including medication side effects, certain health conditions, and lifestyle habits. The Mayo Clinic’s article, “Dry mouth - Symptoms and causes,” provides a comprehensive overview of these causes and potential treatments. Additionally, the National Institute of Dental and Craniofacial Research offers detailed insights in their resource, “Dry Mouth Causes, Symptoms, Diagnosis, Treatment.” If you’re seeking to understand the underlying reasons for dry mouth and explore effective management strategies, these resources offer valuable information.
 Add Row
Add Row  Add
Add 



Write A Comment